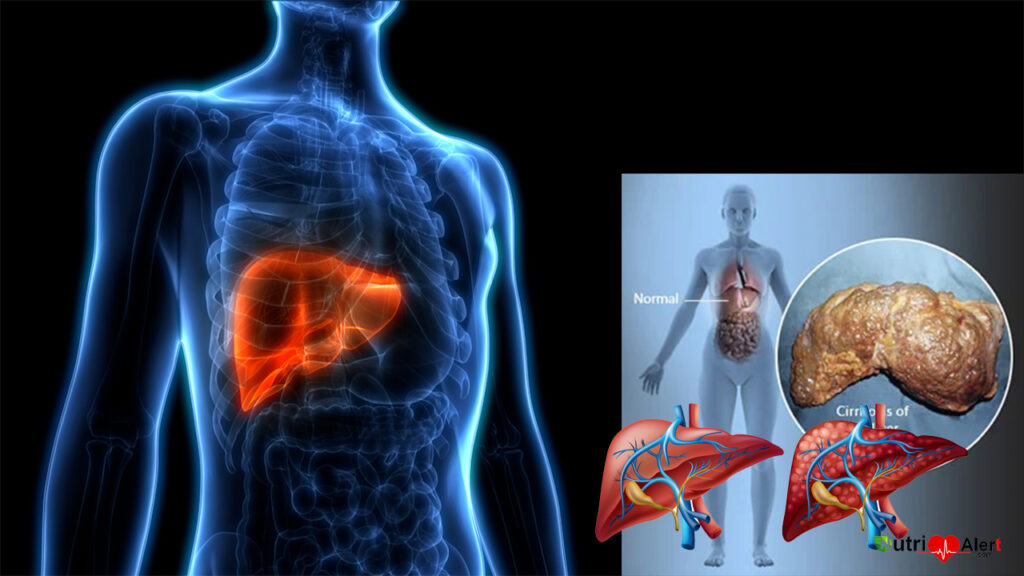
What is cirrhosis of the Liver: Liver cirrhosis is a chronic and progressive liver disease that involves the gradual loss of liver function due to the formation of scar tissue (fibrosis) in the liver. This scarring can disrupt the normal flow of blood through the liver, which can cause a buildup of toxins in the bloodstream and may eventually lead to liver failure.
Liver cirrhosis can be caused by a variety of factors, including long-term alcohol abuse, chronic viral hepatitis, non-alcoholic fatty liver disease (NAFLD), autoimmune disease, and other factors. Some of the common symptoms of liver cirrhosis include fatigue, weakness, loss of appetite, weight loss, abdominal pain, jaundice (yellowing of the skin and eyes), and swelling in the legs or abdomen.
Liver cirrhosis can be diagnosed through blood tests, imaging tests (such as ultrasound or MRI), or a liver biopsy. Treatment for liver cirrhosis may include lifestyle changes, medications, or in some cases, a liver transplant. It is important to seek medical attention if you suspect you may have liver cirrhosis, as early diagnosis and treatment can help prevent further liver damage and improve outcomes.
Foods that affect your Brain and reduce your intelligence | Breast cancer patients can choose a smaller surgery for cure
Liver cirrhosis symptoms:
here are some common symptoms of liver cirrhosis:
- Fatigue and weakness
- Loss of appetite
- Weight loss
- Nausea and vomiting
- Abdominal pain and swelling
- Jaundice (yellowing of the skin and eyes)
- Itchy skin
- Dark urine and pale stools
- Easy bruising and bleeding
- Confusion or difficulty concentrating
- Swelling in the legs or ankles
It’s important to note that not everyone with liver cirrhosis will experience all of these symptoms, and some people may not experience any symptoms at all until the disease has progressed to a more advanced stage. If you have concerns about your liver health, it’s important to speak with a healthcare professional.
There are different types of liver cirrhosis, which can be classified based on their underlying causes:
- Alcoholic cirrhosis: This type of cirrhosis is caused by long-term alcohol abuse.
- Non-alcoholic fatty liver disease (NAFLD) cirrhosis: This type of cirrhosis is caused by the buildup of fat in the liver, often due to obesity, insulin resistance, or metabolic syndrome.
- Chronic viral hepatitis cirrhosis: This type of cirrhosis is caused by long-term infection with the hepatitis B or C virus.
- Autoimmune cirrhosis: This type of cirrhosis is caused by the body’s immune system attacking the liver.
- Biliary cirrhosis: This type of cirrhosis is caused by damage to the bile ducts, which can lead to a buildup of bile in the liver.
- Cryptogenic cirrhosis: This type of cirrhosis occurs when the underlying cause cannot be identified, and it is often referred to as “idiopathic” cirrhosis.
It is important to identify the underlying cause of liver cirrhosis in order to determine the best treatment and prevent further liver damage.
Alcoholic cirrhosis:
Alcoholic cirrhosis is a type of cirrhosis that is caused by chronic alcohol abuse. Drinking alcohol in excess can lead to inflammation and scarring of the liver over time, eventually causing healthy liver tissue to be replaced with scar tissue.
Symptoms of alcoholic cirrhosis are similar to those of other types of cirrhosis and can include fatigue, jaundice, abdominal swelling, and confusion. The severity of symptoms may vary depending on the extent of liver damage.
Diagnosis of alcoholic cirrhosis typically involves blood tests to assess liver function, imaging tests to visualize the liver, and sometimes a liver biopsy to confirm the diagnosis.
The most important treatment for alcoholic cirrhosis is to stop drinking alcohol completely. Additionally, other treatments may be recommended to manage symptoms and prevent complications, such as medications to manage fluid buildup or bleeding, and dietary changes to support liver function.
It’s important to seek medical attention if you are concerned about your alcohol use or are experiencing symptoms of liver disease. With early detection and intervention, it is possible to slow the progression of alcoholic cirrhosis and improve outcomes.
Non-alcoholic fatty liver disease (NAFLD) cirrhosis:
Non-alcoholic fatty liver disease (NAFLD) is a condition in which fat accumulates in the liver, leading to inflammation and damage. In some cases, NAFLD can progress to non-alcoholic steatohepatitis (NASH), which is a more severe form of the condition that can lead to cirrhosis.
NAFLD cirrhosis occurs when the liver has been damaged to the point that healthy liver tissue is replaced with scar tissue. This can lead to liver failure if left untreated. Symptoms of NAFLD cirrhosis are similar to those of other types of cirrhosis and can include fatigue, jaundice, abdominal swelling, and confusion.
Diagnosis of NAFLD cirrhosis typically involves blood tests to assess liver function, imaging tests to visualize the liver, and sometimes a liver biopsy to confirm the diagnosis.
The most important treatment for NAFLD cirrhosis is to manage the underlying condition and prevent further liver damage. This may involve lifestyle changes such as maintaining a healthy weight, following a healthy diet, and getting regular exercise. Medications may also be used to manage symptoms and prevent complications.
In severe cases, liver transplant may be necessary to replace the damaged liver with a healthy one from a donor. It’s important to seek medical attention if you are concerned about your liver health or are experiencing symptoms of liver disease. With early detection and intervention, it is possible to slow the progression of NAFLD cirrhosis and improve outcomes.
Chronic viral hepatitis cirrhosis:
Chronic viral hepatitis cirrhosis is a type of cirrhosis that is caused by chronic infection with certain viruses, including hepatitis B virus (HBV) and hepatitis C virus (HCV). These viruses can cause ongoing inflammation and damage to the liver, eventually leading to the development of cirrhosis.
Symptoms of chronic viral hepatitis cirrhosis are similar to those of other types of cirrhosis and can include fatigue, jaundice, abdominal swelling, and confusion. The severity of symptoms may vary depending on the extent of liver damage.
Diagnosis of chronic viral hepatitis cirrhosis typically involves blood tests to assess liver function and to detect the presence of the virus, as well as imaging tests to visualize the liver and sometimes a liver biopsy to confirm the diagnosis.
The most important treatment for chronic viral hepatitis cirrhosis is to manage the underlying viral infection. This may involve antiviral medications, which can help to slow or stop the progression of liver damage, as well as medications to manage symptoms and prevent complications.
In severe cases, liver transplant may be necessary to replace the damaged liver with a healthy one from a donor. It’s important to seek medical attention if you have been diagnosed with chronic viral hepatitis or are experiencing symptoms of liver disease. With early detection and intervention, it is possible to slow the progression of chronic viral hepatitis cirrhosis and improve outcomes.
Autoimmune cirrhosis:
Autoimmune cirrhosis is a type of cirrhosis that is caused by an autoimmune response in which the body’s immune system mistakenly attacks healthy liver cells. Over time, this can lead to inflammation and damage to the liver, eventually causing healthy liver tissue to be replaced with scar tissue.
Symptoms of autoimmune cirrhosis are similar to those of other types of cirrhosis and can include fatigue, jaundice, abdominal swelling, and confusion. The severity of symptoms may vary depending on the extent of liver damage.
Diagnosis of autoimmune cirrhosis typically involves blood tests to assess liver function and to detect the presence of autoantibodies, which are antibodies produced by the immune system that attack healthy liver cells. Imaging tests may also be used to visualize the liver and sometimes a liver biopsy is performed to confirm the diagnosis.
The most important treatment for autoimmune cirrhosis is to manage the underlying autoimmune condition and prevent further liver damage. This may involve medications to suppress the immune system and reduce inflammation, as well as medications to manage symptoms and prevent complications.
In severe cases, liver transplant may be necessary to replace the damaged liver with a healthy one from a donor. It’s important to seek medical attention if you have been diagnosed with an autoimmune condition or are experiencing symptoms of liver disease. With early detection and intervention, it is possible to slow the progression of autoimmune cirrhosis and improve outcomes.
Biliary cirrhosis:
Biliary cirrhosis, also known as primary biliary cirrhosis (PBC), is a type of cirrhosis that is caused by damage to the small bile ducts within the liver. Bile is a fluid that is produced by the liver to aid in the digestion of fats, and the bile ducts are the small tubes that carry bile out of the liver and into the small intestine. In PBC, damage to the bile ducts leads to a buildup of bile in the liver, which can cause inflammation and scarring over time.
Symptoms of biliary cirrhosis are similar to those of other types of cirrhosis and can include fatigue, jaundice, abdominal swelling, and confusion. Itching is a common symptom of PBC that is not typically seen in other types of cirrhosis. The severity of symptoms may vary depending on the extent of liver damage.
Diagnosis of biliary cirrhosis typically involves blood tests to assess liver function and to detect the presence of specific autoantibodies that are associated with the condition. Imaging tests may also be used to visualize the liver and sometimes a liver biopsy is performed to confirm the diagnosis.
The most important treatment for biliary cirrhosis is to manage the underlying condition and prevent further liver damage. This may involve medications to reduce inflammation and slow the progression of the disease, as well as medications to manage symptoms such as itching. In severe cases, liver transplant may be necessary to replace the damaged liver with a healthy one from a donor.
It’s important to seek medical attention if you are experiencing symptoms of liver disease or have been diagnosed with PBC. With early detection and intervention, it is possible to slow the progression of biliary cirrhosis and improve outcomes.
Cryptogenic cirrhosis:
Cryptogenic cirrhosis is a type of cirrhosis that is characterized by scarring of the liver for which no specific cause can be identified. In other words, it is a type of cirrhosis for which the underlying cause is unknown.
Symptoms of cryptogenic cirrhosis are similar to those of other types of cirrhosis and can include fatigue, jaundice, abdominal swelling, and confusion. The severity of symptoms may vary depending on the extent of liver damage.
Diagnosis of cryptogenic cirrhosis typically involves blood tests to assess liver function, imaging tests to visualize the liver, and sometimes a liver biopsy to confirm the diagnosis. It is important to rule out other potential causes of liver damage, such as viral hepatitis or alcohol abuse, before making a diagnosis of cryptogenic cirrhosis.
The most important treatment for cryptogenic cirrhosis is to manage the underlying condition and prevent further liver damage. This may involve medications to reduce inflammation and slow the progression of the disease, as well as lifestyle changes such as a healthy diet, exercise, and avoiding alcohol and other substances that can damage the liver.
In severe cases, liver transplant may be necessary to replace the damaged liver with a healthy one from a donor. It’s important to seek medical attention if you are experiencing symptoms of liver disease or have been diagnosed with cryptogenic cirrhosis. With early detection and intervention, it is possible to slow the progression of the disease and improve outcomes.
Liver cirrhosis causes:
here are some common causes of liver cirrhosis:
- Long-term alcohol abuse
- Chronic viral hepatitis (hepatitis B or C)
- Non-alcoholic fatty liver disease (NAFLD) is caused by obesity, type 2 diabetes, metabolic syndrome, or high cholesterol
- Autoimmune liver diseases, such as primary biliary cholangitis or autoimmune hepatitis
- Genetic diseases that affect the liver, such as hemochromatosis or Wilson’s disease
- Chronic exposure to environmental toxins, such as arsenic, vinyl chloride, or chloroform
- Biliary tract disorders, such as primary sclerosing cholangitis or biliary atresia
- Some medications, such as methotrexate or amiodarone
It’s important to note that liver cirrhosis can have more than one cause, and some cases of cirrhosis may have no identifiable cause. If you are concerned about your risk of developing liver cirrhosis, speak with your healthcare professional.
Diagnosing cirrhosis of the liver:
here are some common methods used to diagnose cirrhosis of the liver:
- Blood tests to check liver function and detect the presence of viruses that can cause liver damage (such as hepatitis B or C)
- Imaging tests, such as ultrasound, CT scan, or MRI, to visualize the liver and detect any signs of scarring or other abnormalities
- Fibroscan, a non-invasive test that uses ultrasound to measure the stiffness of the liver and determine the extent of scarring
- Liver biopsy, a procedure in which a small sample of liver tissue is removed and examined under a microscope to assess the extent of damage and determine the underlying cause of cirrhosis
It’s important to note that not all people with cirrhosis will require a liver biopsy, and the specific tests used to diagnose cirrhosis may vary depending on the individual case. If you are concerned about your risk of developing cirrhosis or are experiencing symptoms of liver disease, speak with your healthcare professional.
Liver cirrhosis treatment:
Liver cirrhosis can be a serious and potentially life-threatening condition, and the appropriate treatment for an individual with cirrhosis will depend on the underlying cause and the severity of the disease. Here are some common treatments for liver cirrhosis:
- Treating the underlying cause: If cirrhosis is caused by a specific underlying condition such as viral hepatitis, the focus of treatment will be on managing that underlying condition. This may involve antiviral medications or other treatments depending on the cause. Treating the underlying cause of cirrhosis (such as hepatitis B or C)
- Lifestyle changes: Making healthy lifestyle changes can help to prevent further damage to the liver and slow the progression of cirrhosis. This may include avoiding alcohol, maintaining a healthy weight, following a healthy diet, and getting regular exercise.
- Medications: There are a variety of medications that can help to manage symptoms of cirrhosis and prevent complications. For example, diuretics may be used to reduce fluid buildup in the body, beta-blockers may be used to lower the risk of bleeding, and lactulose may be used to help manage confusion or other neurological symptoms.
- Treating complications: Cirrhosis can lead to a variety of complications such as infections, bleeding, or fluid buildup in the abdomen or legs. Treatment for these complications will depend on the specific issue, but may involve antibiotics, endoscopic procedures, or other interventions.
- Liver transplant: In cases where cirrhosis is severe and the liver is no longer functioning properly, a liver transplant may be necessary. This involves replacing the damaged liver with a healthy liver from a donor.
It’s important to note that the appropriate treatment for cirrhosis will depend on the individual case, and treatment may involve a combination of these options. If you are concerned about cirrhosis or have been diagnosed with the condition, it’s important to speak with a healthcare professional to determine the best course of treatment.
Conclusion:
Liver cirrhosis is a serious condition in which healthy liver tissue is replaced with scar tissue, ultimately leading to liver failure. There are a variety of potential causes of cirrhosis, including chronic alcohol abuse, viral hepatitis, and non-alcoholic fatty liver disease, among others.
Symptoms of cirrhosis can include fatigue, jaundice, abdominal swelling, and confusion, among others. Diagnosis typically involves a combination of blood tests, imaging tests, and liver biopsy.
Treatment for cirrhosis will depend on the underlying cause and the severity of the disease, but may include lifestyle changes, medications to manage symptoms and prevent complications, and in some cases, liver transplant.
It’s important to seek medical attention if you are experiencing symptoms of liver disease, as early detection and intervention can help to prevent further damage to the liver and improve outcomes. With proper management, it is possible to slow the progression of cirrhosis and improve quality of life for those living with the condition.