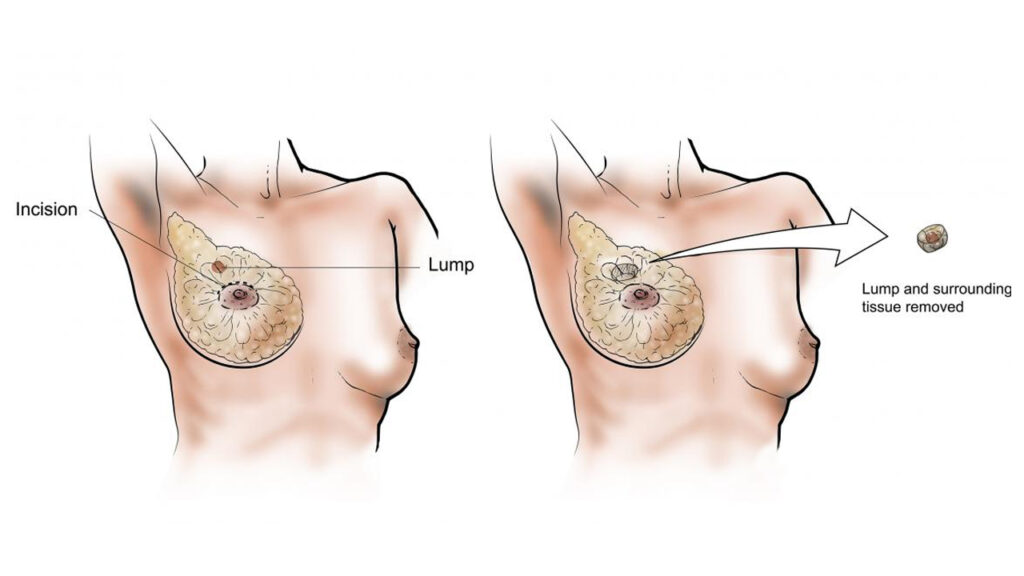
Breast cancer: According to a recent study, many women with two or three breast tumors can survive with lumpectomy surgery rather than having their entire breasts removed.
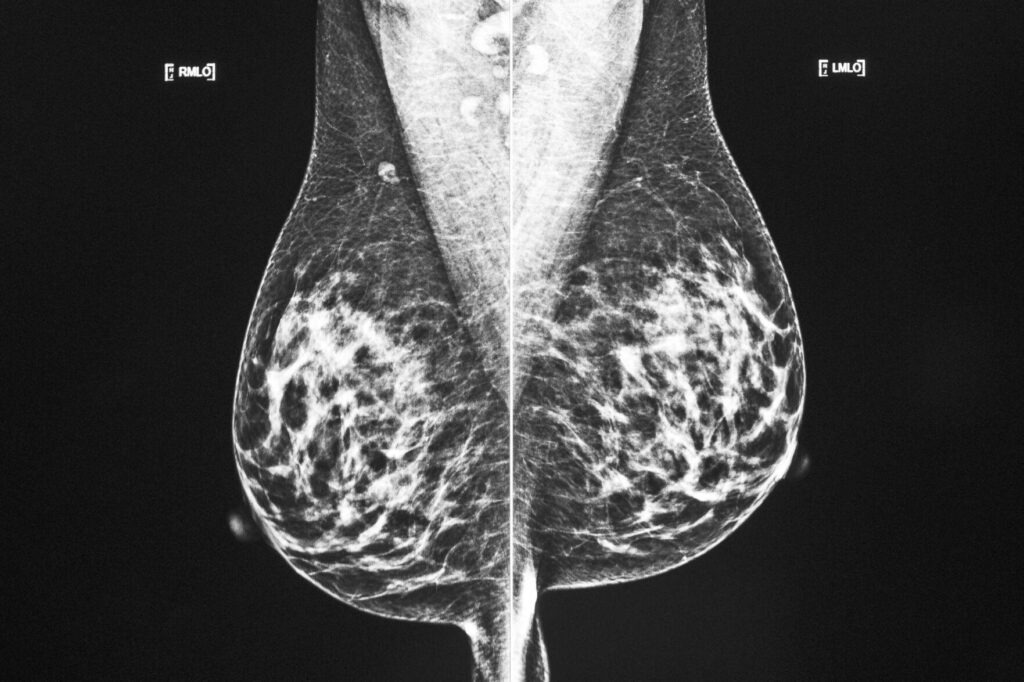
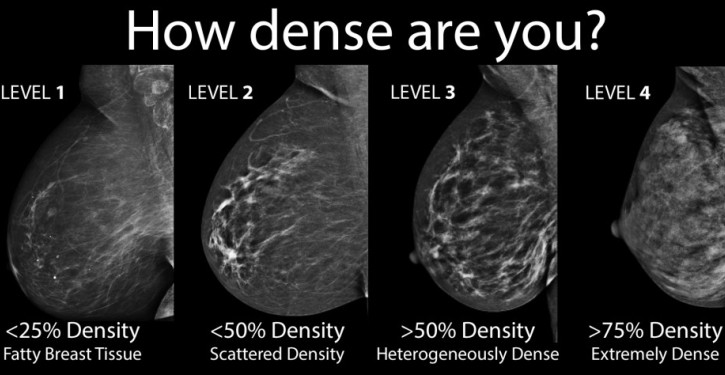
As a result of more sophisticated imaging techniques that can detect microscopic, previously undetectable malignancies, more patients with multiple tumors (Neoplasm) have recently been detected. This indicates that more people are receiving diagnoses for cancer at numerous sites inside the same breast.
In the past, medical professionals would advise mastectomies for these women. Was this orthodoxy still valid, the researchers wondered?
Foods that affect your Brain and reduce your intelligence | How Modern Phones harm your brain at sleeping time
Breast cancer patients can choose lumpectomy
They monitored close to 200 women who underwent lumpectomies and radiotherapy after having two or three tumors removed from one breast. Ages of the patients ranged from 40 years to 87 years. Their tumors had to be less than 5 centimetres in size and separated from one another by 2 to 3 centimetres of healthy breast tissue in order to be eligible for the trial.
Just 3% of individuals with cancer returned after five years, which is comparable to rates from other lumpectomy trials in patients with a single tumor. The National Institutes of Health-funded study was the topic of discussion on Friday at the San Antonio Breast Cancer Symposium.
Dr. John Kiluk, a surgeon at the Moffitt Cancer Center in Tampa, Florida, who was not involved in the study, said “This report drew my interest very immediately.” “Our field has undoubtedly made progress in this regard.”
The benefits of a lumpectomy include a speedier healing time and frequently superior cosmetic outcomes.
According to Dr. Judy Boughey of the Mayo Clinic, who oversaw the research, there were no recommendations for surgery for these individuals, although some clinicians were already suggesting lumpectomy as a choice.
The strategy will increase Breast cancer patients’ comfort level
This will increase their comfort level with that strategy, according to Boughey. “Additionally, I believe it will prompt patients to tell their surgeon that they have two diseased areas. Must I undergo a mastectomy? Can you offer me breast conservation instead?”
Patients were not given a lumpectomy or mastectomy at random in the trial. Better data would have resulted from that, but Boughey claimed that it would be very difficult to locate women who would be ready to participate in a random assignment, rendering such an experiment impracticable.
The results of the study showed that the women who underwent an MRI before surgery fared the best, indicating that MRI scans may enable surgeons to remove cancer more thoroughly.
According to Boughey, the study is a component of a larger research effort targeted at “right-sizing” cancer treatments in order to prevent overtreatment and pointless side effects.
She remarked, “Do we have to throw the kitchen sink at everyone?” “Which patients require each and every treatment option we offer, and which can get by without receiving everything we have to offer? There are adverse effects to every single medication.”